Exploring the experience of pain in haemophilia
Pain in haemophilia has become something of a hot topic – these days, any respectable haemophilia conference will include a session about it on the agenda.
In a recent review, the WHO estimated the prevalence of unspecified pain in adults aged 25+ years across 52 countries at 27.5%[1]. Women, older persons, and rural residents were significantly more likely to report pain.
Estimates of the prevalence of chronic pain in haemophilia vary depending on the definitions used, populations studied and methodology employed. Most seem to suggest that 32-50% of people with haemophilia experience chronic pain.
A few years ago, Haemnet conducted the SO-FIT study[2], looking at physical function in well-treated young men with haemophilia. We included a quality of life tool and were surprised to see that many experienced pain. Like most others, we assumed that pain was limited to older people with a history of poorly treated haemophilia – and we wanted to investigate this further.
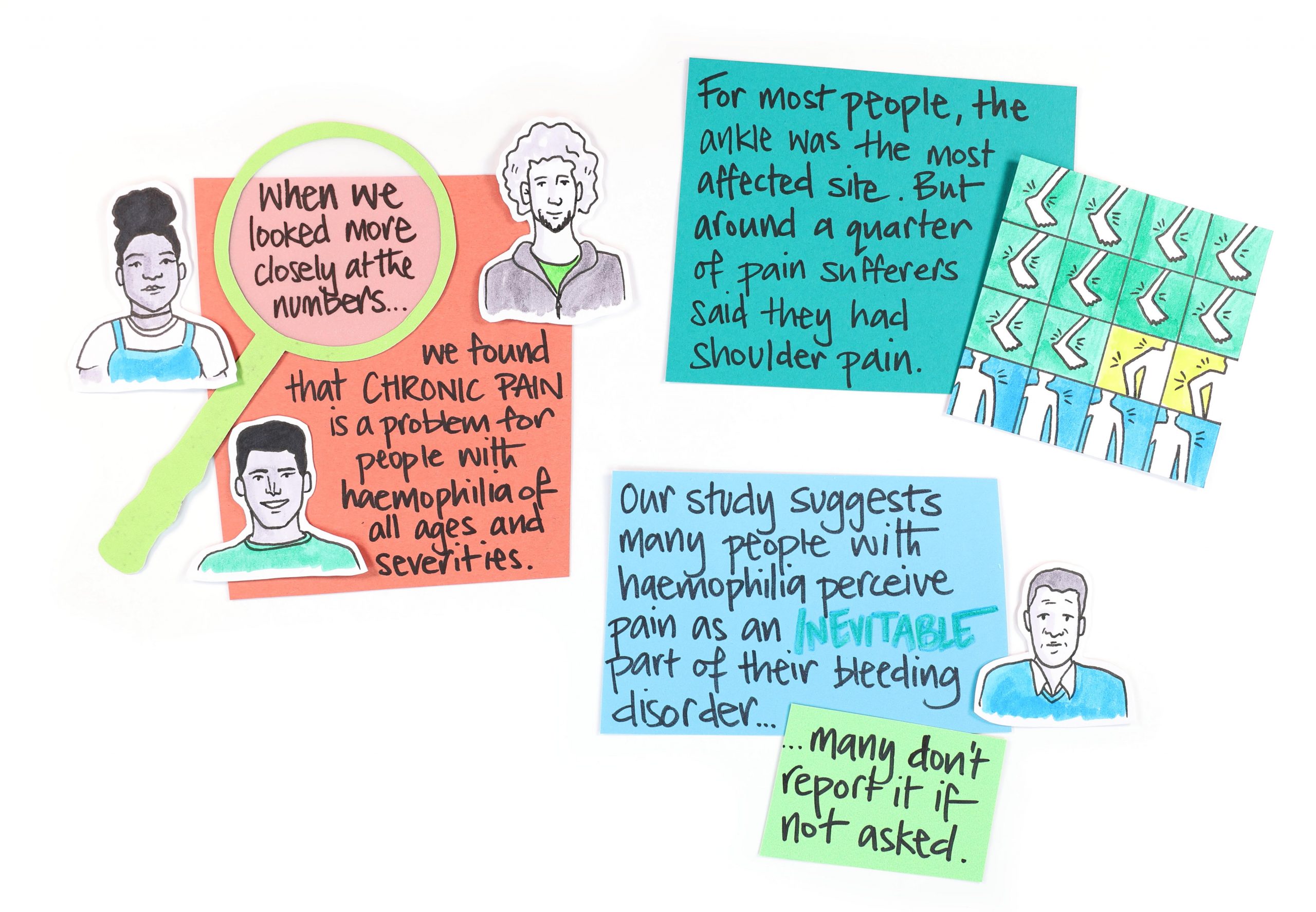
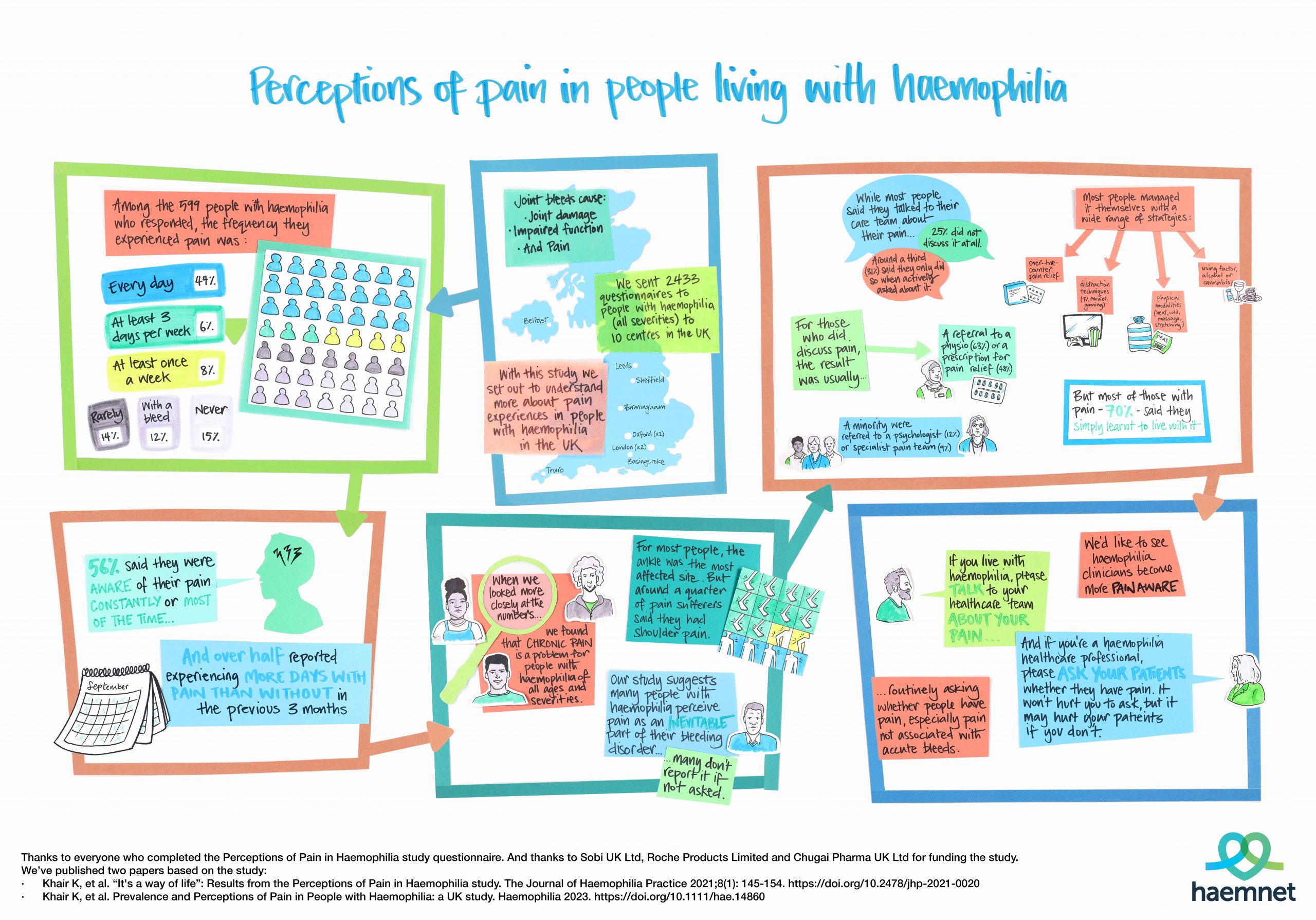
Perceptions of Pain
We devised a study called Perceptions of Pain in Haemophilia[3]. We wanted to look at the experience of pain in men with haemophilia (all severities) in the UK, including what they do to manage it. To gain a holistic view of their real-life experience, we chose a mixed-methods approach.
Our steering committee of people with haemophilia, doctors, nurses, psychologists and physiotherapists developed a questionnaire to capture details of haemophilia and its management. Some questions were selected from existing validated pain and quality of life measures, others were designed to help us understand how people cope with and manage their pain.
To get a good cross-sectional representation of the UK haemophilia population, the questionnaires (and pre-paid return envelopes) were sent out by 10 centres across the country to about one-third of the whole UK haemophilia population.
Responses were totally anonymous, and the study was done with full ethical approval.
Not just about bleeding
We had a near 25% response rate, with questionnaires sent back from over 8% of the UK haemophilia population.
There was a good spread in terms of the age groups represented, though responses were dominated by older age groups. You could argue that this reflects personal experience: assuming those in the older age groups are more likely to experience pain, they may also have been more likely to complete an unsolicited questionnaire dealing with pain.
However, across the age groups we found that people with haemophilia experience a lot of pain in terms of frequency, persistence and awareness. Ankles, knees, and elbows appear to be the most affected joints. The people who responded to our questionnaire were generally pretty well treated – so this pain is not just about bleeding.
“Nobody asks me”
Importantly, we also wanted to know what people actually did about their pain. Most talked to their centre staff about it, but around a quarter of the people we heard from said they don’t talk about pain with their clinicians. And even among those who do, only a third did so if their clinician asked about it. In free text comments, people wrote things like:
“They’re only interested in bleeding episodes”
“It’s never come up”
“I don’t like to moan”
“It’s not bleed pain, so no support given”
“I thought it was just old age”
“I never associated pain with haemophilia”
“Nothing stops it and I have tried everything”
“Nobody asks me”
Many responses indicated that people didn’t associate their pain with haemophilia. But for others, pain was part of their haemophilia. In fact, for most, pain was just something they had “learned to live with”.
An important part of our mixed methods approach to the study was interviewing people to find out about their experience of pain in more depth[4]. In the interviews we conducted, many people told us their social life, work and education were all impacted by pain. Needing to take time off work or school because of pain wasn’t uncommon.
“I’m at college and it’s hard to explain to people why you’re taking so much time off […]
And you’re just there, like, yes, your learning is impacted a hell of a lot, but you need it to rest.”
Time to research pain differently
Our study confirms that pain is a serious problem for many people living with haemophilia. Given the significant impact on quality of life, and the fact that everyone talks about it at conferences, you might think that researchers would be falling over themselves to find the best ways to deal with it. Apparently not.
Of 29,928 studies into pain currently listed on clinicaltrials.gov only 29 deal with haemophilia – that’s 0.01%.
Of 135 studies listed in bleeding disorders, 22 are evaluating pain in some way, usually in the context of joint health in novel haemophilia treatments. Only one is looking specifically at haemophilia pain in all its complexity.
There are no studies looking at pain in other bleeding disorders. And no studies looking at pain in women who live with bleeding disorders.
Isn’t it about time for research into bleeding disorders to be driven by the experiences and priorities of people who live with bleeding disorders?
References
1. Zimmer Z, Fraser K, Grol-Prokopczyk H, Zajacova A. A global study of pain prevalence across 52 countries: examining the role of country-level contextual factors. Pain 2022;163(9):1740-1750. doi: 10.1097/j.pain.0000000000002557.
2. Khair K, Holland M, Bladen M, Griffioen A, McLaughlin P, von Mackensen S; SO-FIT Study Group. Study of physical function in adolescents with haemophilia: The SO-FIT study. Haemophilia 2017; 23(6): 918-925. doi:10.1111/hae.13323.
3. Khair K, McLaughlin P, Roussel, Boyton M, Holland M. Prevalence and Perceptions of Pain in People with Haemophilia: a UK study. Haemophilia 2023. doi: 10.1111/hae.14860. Online ahead of print.
4. Khair K, Kriukow J, Holland M. “It’s a way of life”: Results from the Perceptions of Pain in Haemophilia study. JHaem Pract 2021;8(1): 145-154. doi: 10.2478/jhp-2021-0020.
Other resources
To access our infographic summarising the results of the Perceptions of Pain in Haemophilia study, click here.
Our short animation, John’s Story, explores the experience of pain in a man with severe haemophilia A as told to Haemnet researchers during Project Phoenix. Watch here:
Haemnet’s Director of Research, Dr Kate Khair, discusses pain in haemophilia with haemophilia physiotherapists and pain experts Dr Paul McLaughlin and Prof. Nathalie Roussel in a special two-part episode of Haemcast. Listen here:
- We don’t ask. They don’t tell – Pain and haemophilia (part 1)
- We don’t ask. They don’t tell – Pain and haemophilia (part 2)
About the author
Mike Holland is CEO of Haemnet Ltd.
To find out more about Haemnet’s mixed methods lived experience research and how it enables in-depth insights, email us at research@haemnet.com